Maple Syrup Disease (MSUD) is a serious genetic disorder that needs quick medical help. It affects how the body breaks down proteins, making it hard for families and doctors. Finding and treating this disease is key.
Newborns with MSUD need special tests and fast action. Their urine smells like maple syrup, which is a sign doctors look for. Catching it early can stop serious brain problems.
Genetics play a big part in MSUD. Families with metabolic disorders should watch for genetic tests and early checks. The disease stops the body from breaking down certain amino acids, leading to dangerous protein buildup.
Doctors use many tests to find MSUD. Blood tests, genetic screens, and metabolic tests are important. Parents and doctors must work together to spot symptoms early and start treatment fast.
Understanding Maple Syrup Disease is complex. This intro gives a basic overview. It prepares us for learning more about diagnosing, genetics, and treatments.
Understanding Maple Syrup Disease: An Overview
Maple Syrup Urine Disease (MSUD) is a rare genetic disorder that affects many families. It makes it hard for the body to break down certain amino acids. This creates big challenges for doctors and families.
Testing for MSUD gives us important clues about this condition. It shows how the body’s protein breakdown is affected by enzyme problems. The disease is named after the sweet smell of an affected baby’s urine, like maple syrup.
What Makes MSUD Different from Other Metabolic Disorders
MSUD is unique because of its genetic cause, BCKD Deficiency. It has a few key differences:
- It can’t break down branched-chain amino acids
- Toxic metabolites build up quickly
- It can lead to serious brain problems
- Needs special and quick metabolic care
The History and Discovery of MSUD
The first MSUD cases were reported in the 1950s. Scientists found out how genetics play a role in the disorder. They learned that enzyme problems are key to protein breakdown.
Global Prevalence and Statistics
| Region | Estimated Incidence | Genetic Variation |
|---|---|---|
| North America | 1 in 185,000 births | Multiple genetic mutations |
| Mennonite Populations | 1 in 380 births | Specific founder mutation |
| Global Average | 1 in 250,000 births | Varied genetic backgrounds |
To understand MSUD, we need detailed genetic studies and special tests. These help find out how BCKD Deficiency affects each person.
Early Signs and Symptoms of MSUD
Maple Syrup Urine Disease (MSUD) shows important early signs that need quick medical help. The symptoms start soon after a baby is born. This makes diagnosing MSUD very important for a baby’s health.
Parents and doctors should look out for certain signs of this metabolic disorder. These signs usually show up in the first days or weeks of a baby’s life.
- Distinctive maple syrup-like odor in the baby’s urine and earwax
- Extreme lethargy and decreased muscle tone
- Poor feeding patterns
- Rapid breathing and possible respiratory problems
- Seizures or neurological issues
When babies show these signs, it’s very important to get a diagnosis for maple syrup urine disease. Genetics also play a big part in knowing if a baby might be at risk.
Neurological symptoms can get worse fast. This shows how urgent it is to get medical help right away. Babies with MSUD might face:
- Developmental delays
- Cognitive problems
- Possible brain damage if not treated
Spotting these symptoms early helps doctors start important tests and treatments. This is key for managing this complex metabolic condition.
Maple Syrup Disease Diagnosis: Essential Testing Methods
Diagnosing Maple Syrup Urine Disease (MSUD) needs a detailed approach. This includes several specialized tests. Early detection through these tests can greatly improve patient care and management.
Doctors use many important tests to find and confirm MSUD, mainly in newborns. These tests are key to spotting the metabolic disorder early. This allows for quick action and the right treatment.
Newborn Screening Protocols
Newborn Screening is the first step in finding MSUD. It involves blood tests that check for certain metabolic markers:
- Comprehensive metabolic panel assessment
- Measurement of branched-chain amino acid levels
- Rapid identification of metabolic irregularities
Blood Amino Acid Analysis
Blood amino acid analysis gives deep insights into MSUD’s metabolic issues. It helps doctors understand the biochemical imbalances in patients.
Key parts of this analysis include:
- Quantitative measurement of leucine, isoleucine, and valine levels
- Identification of metabolic pathway disruptions
- Assessment of enzymatic deficiencies
Genetic Testing Procedures
Genetic Testing confirms MSUD by finding specific genetic mutations. This advanced test gives a full view of the genetic factors behind the disorder.
The genetic testing process usually includes:
- Comprehensive DNA sequencing
- Identification of specific gene mutations
- Evaluation of inheritance patterns
Each test is vital for accurately diagnosing and understanding MSUD. This helps doctors create specific treatment plans for patients.
Genetic Factors and Inheritance Patterns
Maple Syrup Urine Disease (MSUD) is a complex genetic disorder. It comes from specific chromosomal mutations. Genetic testing is key to understanding how this rare metabolic condition is passed down.
The disease is caused by mutations in the BCKDHA, BCKDHB, and DBT genes. These genes code for the branched-chain alpha-keto acid dehydrogenase (BCKD) enzyme complex.
- Both parents must carry the genetic mutation
- Each pregnancy has a 25% chance of a child having MSUD
- Carriers usually don’t show symptoms of the disease
BCKD Deficiency is the main genetic cause of MSUD. When this enzyme complex doesn’t work right, the body can’t break down certain amino acids. This leads to dangerous protein buildup.
| Genetic Characteristic | Details |
|---|---|
| Inheritance Pattern | Autosomal Recessive |
| Affected Genes | BCKDHA, BCKDHB, DBT |
| Carrier Probability | 1 in 185 individuals |
Families with a history of MSUD can get genetic testing. This helps them understand their risk. It also helps them make better choices about having children.
The Role of BCKD Deficiency in MSUD
Maple Syrup Urine Disease (MSUD) is caused by a problem with how the body breaks down amino acids. This issue comes from a genetic condition called BCKD Deficiency. It makes it hard for the body to handle certain amino acids, leading to big problems.
The Branched-Chain Ketoacid Dehydrogenase enzyme is key in breaking down proteins. If it doesn’t work right, the body can’t handle some amino acids. This leads to serious metabolic issues.
Understanding Enzyme Function
BCKD Deficiency messes up how the body breaks down three important amino acids:
- Leucine
- Isoleucine
- Valine
This enzyme usually turns these amino acids into energy. But without it working, these amino acids build up. This makes the body toxic.
Metabolic Pathways Affected
The problem caused by BCKD Deficiency affects many body processes. The buildup of amino acids can harm the brain, slow development, and even cause life-threatening crises.
Genetic changes stop the enzyme from working right. This leads to a series of metabolic problems. These need careful medical care to manage.
Types and Classifications of MSUD
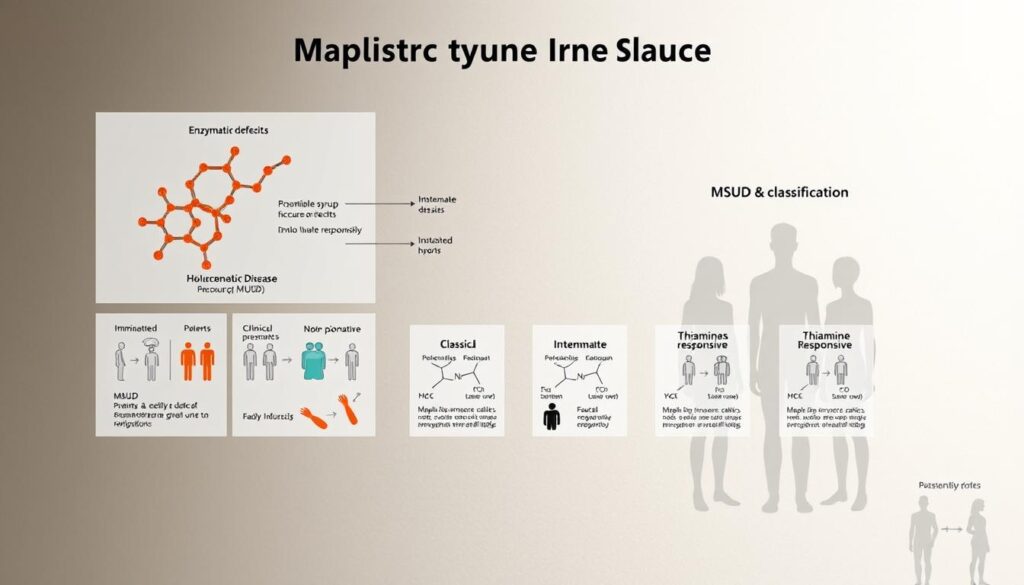
Maple Syrup Disease (MSUD) is not just one condition. It’s a range of metabolic disorders with different types. Each type affects how doctors treat and manage the disease.
The main types of MSUD include:
- Classic MSUD: The most severe form, with a big enzyme deficiency
- Intermediate MSUD: Has partial enzyme function, with milder symptoms
- Intermittent MSUD: A rare form with occasional metabolic issues
- Thiamine-Responsive MSUD: A special type that responds to vitamin supplements
Testing for MSUD is key to figuring out which type someone has. Each type has its own genetic changes that affect how the body breaks down certain amino acids. By identifying the specific type, doctors can tailor treatments to each patient.
Knowing the different types helps doctors create better treatment plans. The severity and genetic details of each type guide the long-term care for those with MSUD.
Early and accurate diagnosis is vital for managing MSUD effectively.
Organic Acid Analysis and Laboratory Testing
Diagnosing Maple Syrup Disease (MSUD) needs advanced lab tests. These tests give important insights into how our bodies work. Organic acid analysis is key to understanding this genetic disorder.
Doctors use top-notch tests to spot and keep an eye on MSUD. These tests mainly look at metabolic markers and amino acid profiles.
Interpreting Test Results
Organic acid analysis checks metabolic byproducts in body fluids. It focuses on:
- Finding odd metabolite levels
- Spotting biochemical issues
- Checking how metabolic pathways work
Monitoring Leucine Levels
Leucine levels are very important in MSUD care. Measuring this amino acid helps doctors:
- Watch metabolic health
- Change diet plans
- Stop brain problems
Organic acid analysis gives a full view of metabolic health. Leucine levels are a main tool for diagnosis and tracking. Lab tests help doctors create specific treatment plans for MSUD patients.
Accurate metabolic screening is key for good MSUD care and patient health.
Clinical Presentation in Infants
Maple Syrup Urine Disease (MSUD) shows clear signs in newborns that need quick action. The diagnosis of Maple Syrup Disease is key in the first weeks of a baby’s life. This is when symptoms show up strongly.
Babies with MSUD have symptoms that show they are in metabolic trouble. A key sign is a sweet smell like maple syrup from their urine and earwax. This smell is a big clue for doctors when they check for Maple syrup urine disease.
- Feeding problems and weak sucking
- Extreme tiredness and weak muscles
- Fast breathing and breathing problems
- Neurological issues like seizures
- A sweet smell from their body
Symptoms can get worse fast and be very serious. Without quick help, brain problems can happen quickly. It’s very important to spot MSUD early and get medical help fast.
Tests for genes and metabolism are key to finding the disease. Blood tests can find high levels of certain amino acids. These are signs of MSUD in babies.
Spotting the disease early through newborn tests can stop brain damage. It also helps babies with MSUD do better in the long run.
Emergency Care and Acute Management
When a patient with Maple Syrup Urine Disease (MSUD) has a metabolic crisis, quick medical help is vital. Testing for MSUD and watching leucine levels closely are key parts of emergency care. They help avoid serious problems.
Doctors have a fast plan for MSUD emergencies. It aims to keep the patient stable and lower harmful amino acid levels.
Critical Care Intervention Strategies
Handling MSUD emergencies needs a detailed plan. It covers many areas of metabolic trouble:
- Immediate blood chemistry assessment
- Rapid leucine level evaluation
- Electrolyte balance correction
- Nutritional support modifications
Stabilization Techniques
Special medical steps are key for managing MSUD crises. They aim to quickly lower amino acid levels with precise methods.
| Intervention Method | Primary Purpose | Expected Outcome |
|---|---|---|
| Hemodialysis | Remove excess amino acids | Rapid leucine level reduction |
| Specialized IV Nutrition | Metabolic crisis management | Prevent neurological damage |
| Continuous Amino Acid Monitoring | Track metabolic changes | Adjust treatment in real-time |
Prompt recognition and aggressive treatment are essential in preventing permanent neurological damage during MSUD metabolic crises.
The success of emergency care depends on teamwork. It needs fast tests, special diets, and constant monitoring of metabolism.
Long-term Treatment Strategies
Managing Maple Syrup Disease (MSUD) is a lifelong journey. It starts with understanding the complex nature of BCKD Deficiency. Then, it involves creating care plans that meet the unique needs of each patient.
The main goals of long-term treatment are to prevent metabolic crises and support growth. Healthcare teams create personalized plans. These plans include:
- Regular metabolic monitoring
- Strict dietary management
- Specialized nutritional supplementation
- Genetic counseling
- Ongoing medical surveillance
Nutritional intervention is key in managing MSUD. Patients need the right amount of protein to avoid amino acid buildup. This ensures they get enough nutrients for growth.
| Treatment Component | Key Objectives | Frequency |
|---|---|---|
| Amino Acid Level Monitoring | Prevent metabolic decompensation | Every 2-4 weeks |
| Dietary Management | Control protein intake | Continuous |
| Supplemental Nutrition | Ensure balanced nutrient intake | Daily |
Successful long-term management requires a multidisciplinary approach. Patients benefit from a team effort. This team includes metabolic specialists, nutritionists, and genetic counselors.
Early intervention and consistent management are key to improving quality of life for individuals with Maple Syrup Disease.
New medical technologies offer hope for better treatments. Research aims to find more precise ways to manage BCKD Deficiency. This could lead to better outcomes for patients.
Dietary Management and Restrictions
Managing Maple Syrup Urine Disease (MSUD) needs a well-thought-out diet plan. This plan tackles the challenges of BCKD Deficiency head-on. Patients must keep a close eye on what they eat to avoid serious health problems.
The main aim of diet management is to control Leucine Levels and stop metabolic crises. It involves watching protein intake closely and monitoring metabolism regularly.
Meal Planning Guidelines
Good meal planning for MSUD patients needs a lot of nutritional knowledge. It’s important to pick ingredients carefully. Key points include:
- Limiting branched-chain amino acids
- Measuring protein accurately
- Monitoring metabolism often
- Calculating nutrients individually
Supplementation Requirements
Special nutritional supplements are vital for MSUD management. They help keep nutrient levels right and avoid metabolic risks.
- Medical protein substitutes
- Essential amino acid mixtures
- Vitamin and mineral supplements
- Metabolic formula replacements
Nutrition experts suggest working with metabolic dietitians. They help create diet plans that meet individual needs. This ensures patients grow and develop well.
Precise nutritional management is key to preventing serious metabolic complications in MSUD patients.
Complications and Prevention Methods
Maple Syrup Disease (MSUD) is a serious health issue that needs careful handling. Knowing the possible complications helps in diagnosing and testing for MSUD.
People with MSUD face serious health risks. These risks need quick medical action:
- Neurological damage from high amino acid levels
- Metabolic crisis that could harm the brain
- Developmental delays
- Cognitive impairment
To avoid these problems, a detailed plan is needed. Early detection through thorough MSUD testing is key to lowering health risks.
Important prevention steps include:
- Regular blood amino acid checks
- Strict control of dietary protein
- Quick medical help during metabolic stress
- Regular checks on the nervous system
Doctors suggest strong management to stop brain damage. Special metabolic clinics offer focused care. This care greatly lowers the chance of serious problems from MSUD.
“Proactive management is the cornerstone of successful MSUD treatment” – Metabolic Disease Specialists
Genetic counseling and new testing methods help families deal with risks. This ensures better health for those with this complex metabolic disorder.
Living with MSUD: Daily Considerations
Managing Maple syrup urine disease needs a lot of daily planning. It helps both individuals and families. Living with this rare metabolic disorder means always being careful and keeping an eye on Leucine Levels. It also means building strong support networks.
People with MSUD face big challenges. They need personal plans to keep their lives good. Key parts of managing it well include:
- Strict dietary management
- Regular medical monitoring
- Emotional support systems
- Educational resource engagement
Quality of Life Considerations
Every day with MSUD means watching what you eat and keeping your body balanced. Patients must track their protein intake and stick to special diets. Getting emotional support is also key for dealing with the ups and downs of life with MSUD.
“Knowledge and preparation are the most powerful tools in managing MSUD daily” – Metabolic Disease Specialist
Support Systems and Resources
Having a strong support network is vital for those with Maple syrup urine disease. There are many resources available:
- Genetic counseling services
- Patient support groups
- Metabolic disorder clinics
- Online community forums
Today, advanced medical centers have programs for MSUD management. These programs help patients find ways to stay healthy and well for a long time.
Future Treatment Developments
Medical researchers are making big steps in treating BCKD Deficiency. They are working on new ways to manage Maple Syrup Urine Disease (MSUD). These new methods aim to fix the problem at the root, which is the Branched-Chain Ketoacid Dehydrogenase enzyme.
Several new research paths are being explored for breakthrough treatments:
- Gene Therapy Interventions
- Advanced Enzyme Replacement Strategies
- Precision Metabolic Modifications
- Personalized Nutritional Approaches
Scientists are creating advanced genetic methods to fix the metabolic pathway issues caused by BCKD Deficiency. Experimental gene editing technologies are showing great promise in tackling this complex metabolic disorder.
| Treatment Approach | Potential Impact | Current Research Stage |
|---|---|---|
| CRISPR Gene Editing | Direct Genetic Correction | Preclinical Trials |
| Enzyme Replacement Therapy | Metabolic Function Restoration | Early Clinical Investigations |
| Targeted Nutritional Interventions | Metabolic Balance Optimization | Advanced Research Phase |
The ultimate goal of these new methods is to change MSUD from a tough genetic disorder to a manageable one. The latest research is constantly expanding what’s possible in treating Branched-Chain Ketoacid Dehydrogenase-related metabolic issues.
Impact on Family and Caregivers

Maple Syrup Disease Diagnosis is tough for families. It brings big challenges that go beyond just medical care. Caregivers face emotional and practical hurdles.
The emotional toll of MSUD testing and care is huge. Families deal with:
- Emotional stress from constant medical checks
- Financial worries from expensive treatments
- Complex daily care needs
- Genetic counseling might be needed
Support systems are key for families with MSUD. Professional help and special groups offer vital resources and emotional support.
| Family Support Aspect | Key Considerations |
|---|---|
| Emotional Support | Counseling, peer support groups, mental health resources |
| Financial Resources | Medical insurance, disability support, specialized care funding |
| Educational Needs | Genetic counseling, medical training, school accommodation plans |
MSUD testing needs families to learn a lot. Knowing about genetics and long-term care helps them care better.
“Knowledge and support are the most powerful tools for families facing rare genetic conditions.”
Building resilience is vital for families with Maple Syrup Disease. With the right help, support, and care, families can live better lives.
Conclusion
Maple Syrup Disease (MSUD) is a complex genetic disorder that needs careful medical attention. Understanding it involves genetic testing, metabolic screening, and advanced lab work. Early detection is key to avoiding serious problems and managing the disease well.
Doctors have made big steps in diagnosing Maple Syrup urine disease. Newborn screening, precise genetic tests, and detailed metabolic assessments help doctors act fast. These methods give families the tools they need to manage this rare condition.
Research is growing our knowledge of MSUD’s genetic aspects and new treatments. Special diets, constant medical checks, and new therapies offer hope for better care. Families facing this condition can find help through medical resources, genetic counseling, and metabolic health experts.
Even with challenges, medical science keeps moving forward. The work of researchers, geneticists, and doctors shows the need for ongoing research and tailored care for MSUD.